Connie Hanafy should have been celebrating freedom. After four years of struggling with complex regional pain syndrome, when hyperactive nerves caused her near-constant agony, Hanafy had her right leg amputated below the knee.
Hanafy wanted to return to her athletic lifestyle, playing soccer, surfing and riding horses like when she was growing up in Delran. Her insurance company had other ideas.
Hanafy was able to get a prosthesis so she could walk again. But a running blade? Something she could use to jump into a pool, lake or the Jersey Shore breakers? Or to smoothly kick a soccer ball with her two daughters?
Absolutely not.
That made Hanafy’s disappointment shift to anger.
She already knew the sobering Centers for Disease Control and Prevention statistics. Nearly one in four Americans is living with a disability, about 14% of which impact mobility. Nearly half of those adults with disabilities get no aerobic physical activity.
Hanafy likened the lack of coverage for activity-specific prostheses to how insurance companies handle Type 2 diabetes, which is frequently linked with obesity. Diabetes treatment is covered, but Hanafy doesn’t think there’s enough incentive to help improve someone’s lifestyle before she gets sick.
“You should be treated mind, body and soul as a whole,” said Hanafy, a 37-year-old single mom in Sewell who works with hospice patients.
“Having a limb difference, I don’t want to deal with it. I want to do what I want to do without having a $50,000 (specialized) prosthetic leg and paying out of pocket for it because it’s deemed not medically necessary. It is necessary.”
Though most employer-sponsored and Affordable Care Act plans include “medically necessary” prosthetic devices in their Essential Health Benefits, that coverage is not universally available. Medicaid skips those benefits in states like Oklahoma, Texas and Mississippi. Medicare Part B — which covers durable medical equipment, a category that includes canes and walkers as well as prostheses — requires patients to pay 20% of the cost, which is approximately $5,000 for a basic lower leg.
“If the device(s) are determined to be medically necessary based on a diagnosis by a doctor or other licensed practitioner, they can be covered. It’s case-by-case depending on the situation,” New Jersey Department of Human Services spokesman Tom Hester said via email.
“Medicaid and Medicare cover specialty equipment to support activities of daily living. Medical equipment required exclusively for sports would not be covered by either program.”
Applying for assistance from a nonprofit is not nearly as easy as shopping at a sporting goods store. But as Hanafy and thousands of others have learned, help is available.
Challenged Athletes Foundation, one of the largest nonprofits, gave out $6.2 million in spring 2022. Some 3,250 recipients spanned 83 sports and activities — skiing, wheelchair basketball, fly fishing.
Applications are accepted in the fall, and award notifications go out in late March. Money is then distributed, so adaptive equipment can be ordered and fitted — or coaching and travel booked.
Hanafy went another way, obtaining a grant for a running prosthesis from the Move for Jenn Foundation. She ordered her specialized leg from Levitate, a Copenhagen-based manufacturer that sells prostheses direct to consumer.
Montville teen receives prosthetic hand from paralympian’s nonprofit
Alex Manna, 16, from Montville, received a prosthetic hand funded by Born to Run, a nonprofit founded by Paralympian Noelle Lambert.
Michael Karas, NorthJersey.com
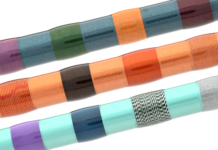
Levitate sells fiberglass running blades for about $2,000 – far less than larger manufacturers like Ossür, which charges $3,500 for a basic below-the-knee foot and more than double that for an above-the-knee amputee. Specialized equipment to run, lift weights and do other physical activity costs tens of thousands of dollars, none of which is covered by insurance.
“No matter where you look in the world, the answer is the same. Recreational equipment is not seen as a right. It’s not deemed necessary,” said Lasse Werner Madsen, who created Levitate three years ago after he faced challenges getting a sports prosthesis.
“You can go down to Dick’s Sporting Goods and buy an entry-level carbon bicycle, but you cannot buy the equipment you need to run. For me that’s not equal. Here’s an underserved need.”
Amputee Coalition is working to further the 2020 Triple A Study Act, which calls for the Government Accountability Office to study health insurance and other coverage for assistive technologies, like prostheses. Meanwhile, the American Orthotic and Prosthetic Association is lobbying Congress to increase coverage for both basic and adaptive prostheses.
In March 2021, Rep. Mike Thompson, a Democrat from northern California, introduced the Medicare Orthotic and Prosthetic Patient-Centered Care Act, which would separate prostheses from other medical equipment — making it easier for medical professionals to get proper payment for the many necessary adjustments.
Mark Warner (D-VA) introduced the Senate version in July, with five bipartisan co-sponsors including Tammy Duckworth (D-Ill.), a U.S. Army veteran and the first bilateral amputee in Congress.
The bills appear to be stalled in committee.
Every state has an insurance program for children up to age 18. However, only one state legislature — Maine — has added activity-specific prostheses to insurance coverage.
“What is it that makes me disabled?” asked Nicole Ver Kuilen, the American Orthotic and Prosthetic Association’s public engagement manager.
“Is it that I’m missing my foot? Or is it these outdated policies that keep me from being able to live an active life?”
Christie Rogero of Voorhees didn’t become an athlete until after her left leg was amputated.
Rogero was waiting for a traffic light to change as she headed from her Philadelphia office to an animal adoption center. As one car went through the intersection, another one sped toward it, didn’t stop and T-boned the car that had right-of-way. That car went careening toward Rogero, and only a light pole prevented it from crushing her against a building.
The nerves in both her legs were shredded. Flesh had to be held together with pins and plates.

Courtesy of Kelly Worrell
Efforts to save Rogero’s left leg went on for about a year. Finally, it was clear: The leg would have to be amputated above the knee. Rogero got a prosthesis a few months later, and quickly learned it’s stronger than her own reconstructed flesh and blood.
The lifelong theater enthusiast was coaxed to attend a handcycling clinic sponsored by a local nonprofit. Rogero took to it immediately.
Usually lower to the ground, handcycles are powered with the arms instead of legs.
But at $3,500 for a basic model, handcycles are also far more expensive than ordinary road bikes. Rogero had to return the bike at the end of each event. Rogero has applied for a grant from the Challenged Athletes Foundation to buy her own. A decision is expected in late March.
“Now that I’ve found something I’m good at and I enjoy, I want to be able to do it much more often,” said Rogero, the director of animal-welfare nonprofit Jackson Galaxy Project. “If I get this grant, I’ll be able to get the bike and keep it at home. It’s a freedom I didn’t know I was missing until I got on the bike and went flying down the road.”
Rogero and Connie Hanafy, both South Jersey residents, have become friends — and each other’s fans.
Eight months after having her right leg amputated below the knee, Hanafy did her first mile run, then a 5K obstacle course in a downpour. In July 2022, she was one of 27 paratriathletes out of 1,500 people who dove into the Hudson River swim leg of the New York City Triathlon.
“Being an athlete again as an adult, I never considered it. Being an athlete on one leg, I sure as hell never considered that,” Hanafy said.
“Normal people would look at me and say, ‘How are you doing this? You don’t have a leg.’ They look at people who have differences as a deterrent from doing something a normal, able-bodied person can do. We just want to show people we’re no different than you. We just might have to do things a little differently. I can still run. It’s just a little bit different than you. I can still swim. It’s just a little bit different than you. I can still bike. It’s just a little bit different than you. To be able to do something you never thought you could ever do, it’s life changing. I was hooked immediately.”
Receiving a grant to use toward a prosthesis – or even a prosthesis direct from a manufacturer like Ossür – isn’t the end of the story. A prosthetist still needs to make the socket — which fits around one’s residual limb and attaches to the prosthesis — and configure the device specifically for the user.
Hanafy’s donated running blade may not be sufficient for the rigors of her new schedule. Even the socket that connects Hanafy’s prosthesis to her residual limb — nicknamed “Mr. Stumpleton”— no longer fits due to her changing body.
Hanafy has been through three sockets in her first year as an amputee. She has to wait, adjust and deal with unnecessary physical and mental irritation until her insurance company will cover another new one.
“You should be able to get up every morning and have the ability, and whatever you need, to go run,” Hanafy said. “It’s part of your quality of life. It’s part of helping you become or stay a healthy person, to be active and not be limited by your prostheses.”
Jane Havsy is a storyteller for the Daily Record and DailyRecord.com, part of the USA TODAY Network. For full access to live scores, breaking news and analysis, subscribe today.
Want to share your story with me?
Email: JHavsy@gannett.com
Twitter: @dailyrecordspts
Published
Updated
Credit: Source link